Benzodiazepines are central nervous system depressants frequently employed to relieve anxiety, sleeplessness, and epileptic seizures. Benzodiazepines are a class of psychoactive drugs that were initially developed to treat anxiety or insomnia, and they are one of the most frequently prescribed medicines in the country. Benzos are available under various brand names, including Valium, Xanax, and Klonopin, and there are many different types.
The primary distinction between these medicines is the length of time they remain active in the body. Benzos are frequently abused for their calming and pleasurable effects, and Benzos, even when used at appropriate dosages, can induce physical dependence and withdrawal in some individuals.
Arcsfl is one of the best health care providers. Benzodiazepines are a class of drugs that are prescribed to treat anxiety disorders and insomnia. They are also used as a sedative or muscle relaxant in some cases. These drugs can cause addiction, however, and long-term use is associated with increased risks of developing memory problems, depression, and other problems. The drugs work by binding to receptors in the brain that produce a calming effect.
Benzodiazepine use in addiction treatment retention, and opioid withdrawal.
Benzodiazepines can be abused by individuals who take them for nonmedical purposes. Abusers may take them to feel relaxed or calm. Medical knowledge take them to self-medicate for depression or anxiety. When taken in large doses, benzodiazepines can cause sedation and amnesia. Some abusers take these drugs to get high.
Gradual dose reduction is a process of gradually decreasing the dosage of medication in order to reduce side effects without stopping the medication. The goal is to minimize the side effects while maintaining the beneficial effects of the medication.
Clinical psychiatry is the branch of medicine that deals with mental health and behavior. It is also known as psychiatry. Treatment alternatives are different ways to treat psychiatric disorders that are not considered traditional methods. For example, some people with schizophrenia use alternative treatments, such as meditation, yoga, and dietary supplements.
Outline of Benzodiazepine Withdrawal
The benzodiazepine abuse has spread. From 1996 to 2013, the number of individuals getting benzo prescriptions increased by 67 percent. Benzodiazepine dependence has risen among people of all ages, from teenagers to the elderly. According to estimates, 500,000 individuals in the United States were victims of drug abuse or dependent on sedative medications in 2016.
Benzodiazepines are habit-forming, and anyone who uses them daily can build up tolerance and dependence.
When you are physically reliant on a drug, it implies that your body cannot function properly without it. You will get withdrawal symptoms if you stop or reduce your dosage dramatically.
It’s not easy, nor is it safe to stop taking benzos suddenly. For several weeks, you may expect to be anxious and irritable, and you could become irritated and hypersensitive to your surroundings. Acute insomnia is also typical. During the first week of addiction treatment, you can anticipate physical symptoms, including headaches and hand tremors.
It’s possible to taper down your dosage gradually to minimize severe symptoms that come and go in cycles. If you’ve been using benzos for longer than six months, stopping abruptly may cause grand mal seizures and delirium. It’s essential for family members to consult with your doctor or healthcare professional throughout the withdrawal process.
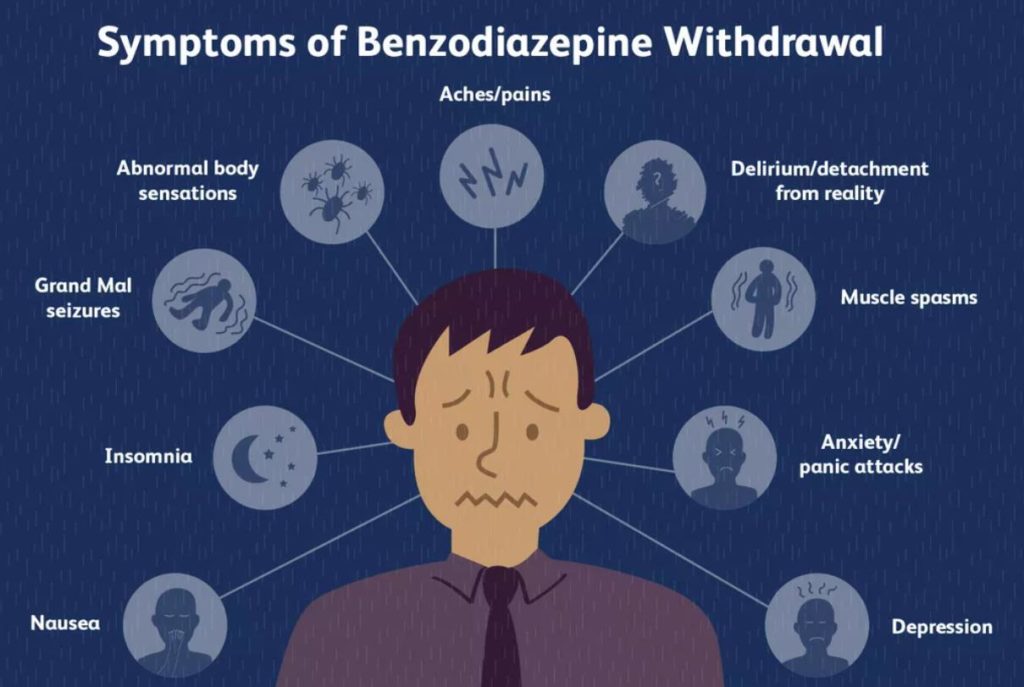
Benzodiazepine Withdrawal Symptoms from Substance Abuse
Even on tiny, therapeutic doses, mind-altering substances such as benzos may produce withdrawal symptoms in some users. When people quit benzo usage abruptly, around 40% of those taking it for longer than six months experience moderate to severe withdrawal symptoms, and the other 60% experience milder symptoms.
Specific factors of benzodiazepine dependence influence the severity of withdrawal symptoms, such as your current dose, how long you’ve been taking it, whether you take more than one benzo, whether you take other sedating drugs, any substance use issues, whether you are quitting more than one substance at a time.
The time it takes for you to quit taking benzodiazepines is determined by the type of drug you are on. Short-acting medicines like alprazolam (Xanax) and lorazepam (Ativan) leave the body more quickly, which means withdrawal can occur in as little as eight to 12 hours.
The half-life of midazolam is shorter than other benzodiazepines, which means it leaves the system sooner. Longer-acting benzos, such as clonazepam (Klonopin), can stay in the body for days or even weeks before effects begin.
Anxiety, Insomnia, Irritability, Restlessness, Nervousness, Hand tremors and spasms, Muscle cramps and spasms, Headache, Sweating, a racing pulse, hyperventilation, nausea or vomiting, pains and aches, Abnormal bodily experiences (skin-crawling, goosebumps), sadness, difficulties with attention and memory, visual disturbances (flashes of light or blurred vision), auditory, tactile, or visual hallucinations, feelings of unreality, delirium Grand mal seizures.
According to the American Psychiatric Association (APA), short-acting benzo withdrawal peaks on the second day and decline by the fourth or fifth day, according to American Psychiatric Association (APA). Some people, on the other hand, report that they continue for several weeks.
Extended withdrawal is a potentially serious symptom that can manifest itself in different ways. According to estimates, 10 to 25 percent of long-term benzo users experience protracted withdrawal. Protracted Withdrawal Syndrome is a long-term withdrawal illness that may come and go for several months.
The symptoms of a protracted withdrawal will be milder than those experienced during acute withdrawal and can persist for weeks at a time. Prolonged quitting rarely lasts more than a year.
Human services are the work of providing assistance to people who have difficulties or need help. These may include helping people in prison, assisting people with mental health problems, providing care to children in orphanages, or helping people who are homeless.
Diseases of the nervous system are diseases that affect the brain, spinal cord, and nerves. They can be caused by injury, infection, genetic disorders, or other conditions. Diseases of the nervous system are also known as neurological diseases.
The Diagnostic and Statistical Manual of Mental Disorders (DSM) is a diagnostic manual published by the American Psychiatric Association. It is used by mental health professionals to classify mental disorders. The DSM is the standard reference for classifying mental disorders.
Must Read: Drugs You Can Get Addicted To
Recognizing A Benzodiazepine Addiction
Benzodiazepine addiction can occur without users or loved ones recognizing anything is wrong. Even when the medicines are taken responsibly within a doctor-prescribed “safe window,” Benzodiazepine addiction might develop. When a medical prescription has run out, or a user begins looking for more powerful effects, strange actions, or indications that they are addicted to benzodiazepines, these are signs of addiction.
Benzodiazepines are drugs used to treat anxiety and insomnia. They are also used to treat panic attacks and other forms of anxiety. They work by increasing the effects of the neurotransmitter GABA in the brain. GABA is an inhibitory neurotransmitter that reduces the activity of neurons. By increasing the amount of GABA in the brain, benzodiazepines can reduce anxiety. Benzodiazepines are sometimes called “benzos” or “benzo” for short.
Benzodiazepines are sedative-hypnotic drugs that are used to treat anxiety and insomnia. The most common benzodiazepines are triazolam (Halcion), temazepam (Restoril), alprazolam (Xanax), lorazepam (Ativan), and diazepam (Valium).
A community-based organization is an organization that works with the community to improve the quality of life for individuals with a mental health condition. For example, a community-based organization might offer support groups for people with a specific type of mental health condition. These groups are often run by people who have a personal connection to the condition.
Mental health conditions are illnesses or problems with the mind. They can include anxiety, depression, bipolar disorder, and schizophrenia. Many mental health conditions are chronic, meaning they can last a long time. Mental health conditions are often treated with medication.
Maintenance treatment is a type of treatment that is used to prevent relapse of a mental health condition. For example, if someone has been diagnosed with depression, the goal of maintenance treatment is to keep them from getting depressed again. The person will be prescribed medication and therapy. If the person is not taking their medication correctly, their doctor will work with them to correct the problem.
Involvement in a Benzodiazepine Issue
The initial step is to acknowledge a loved one’s Benzodiazepine addiction, which must be followed by discussing it with them and devising a strategy to assist. Despite their struggle to quit taking the drug, many individuals cannot recognize that they have an addiction. They may refuse the medical treatment they genuinely require, and they might claim that they don’t need to go to rehab for Xanax, for example. It’s critical to express your concerns in a manner that is both polite and firm.
Coping with Benzodiazepine Withdrawal
The easiest approach to quit benzos is to have your doctor taper down your drug dosage instead of stopping it. Tapering involves gradually reducing the amount you take over a few weeks or months.
It is possible to taper your dosage on your own, but it’s recommended that you consult a doctor. Depending on the benzodiazepine you’re currently taking, your doctor may want to change you to a different one before your taper begins. With too many ups and downs, short-acting benzos make withdrawal difficult. The majority of long-acting benzos are diazepam, which is the most frequent option for dose reduction.
There is no one-size-fits-all tapering plan for you to follow, and your doctor will develop a personalized taper strategy based on your current dose and specific circumstances. Some people complete rapidly, finishing in two to three weeks, and others take months or even years to taper.
You may still have some of the withdrawal during your taper, which can happen after each dosage reduction.
If your discomfort becomes severe, your doctor may temporarily or gradually slow down the taper. Most doctors choose not to reverse the taper and instead boost the dose in response to withdrawal.
It helps to have a fallback strategy for coping with anxiety if you’re going through a breakthrough episode. Cognitive-behavioral therapy, Meditation, Mindfulness instruction, and physical activity are all beneficial techniques.
Must Read: How Long Do Benzos Stay in Urine
Benzodiazepine Withdrawal and Precautions
The abrupt termination of Benzodiazepine therapy can be hazardous if not properly dealt with. There’s a chance that individuals who quit benzos abruptly might have a deadly grand mal seizure. If you taper off Benzo medications, you run the danger of suffering from delirium and hallucinations, which may lead to losing touch with reality—an unpleasant and dangerous experience.
On your own, some medications are safe to quit, but benzodiazepines are not. 4 Benzodiazepines, on the other hand, do not imply that you will require in-patient care. Most people do well with a gradual reduction of their benzos at home using the support of their general practitioner or psychiatrist. You should regularly keep in touch with your doctor during the tapering process, either by phone or in person.
Different individuals and circumstances will require varying dosages of medication, which your doctor may consider it prudent to give in tiny portions at a time. This will prevent you from changing the taper, but frequent trips to the pharmacy may be unavoidable.
Some people, such as those with a history of complicated withdrawal, seizures, or severe mental illness, might do better in an in-patient setting. Living at a detox facility or hospital for several weeks may involve living there continuously and getting medical monitoring and psychological assistance.
Quitting benzos can exacerbate psychiatric problems, which might include panic attacks, obsessive-compulsive symptoms, PTSD symptoms, severe anxiety, intrusive thoughts, and depression.
In-patient treatment might be expensive, depending on the facility, but it is often covered by insurance.
If you’re pregnant or considering becoming one, see your OBGYN or psychiatrist immediately about your intentions. Benzodiazepine use during pregnancy has some risks. However, any withdrawal throughout pregnancy has its dangers. Your physician can assist you in weighing the prospective drawbacks and advantages of using benzodiazepines while pregnant.
Long-Term Treatment for Benzodiazepine Withdrawal
Longer-term treatment after quitting benzo use will be determined by your motives for taking the drugs in the first place, as well as your motivation to stop. You’ll need a different strategy for managing your condition if you have a psychiatric problem treated with benzos, and this is generally made up of both therapy and pharmaceutical assistance.
If you’re quitting benzos because you were misusing them or couldn’t control your usage, you’ll likely need additional substance abuse therapy. This is especially true if you’re giving up other drugs, such as alcohol or opioids.
Psychotherapy may assist you in determining the underlying cause of your substance abuse issues. It can also teach you how to identify psychological stimuli that might lead you to relapse so that you can avoid them in the future.
Your prescription doctor is the most excellent resource in your effort to withdraw from benzos. However, if you prefer someone else, any family physician or psychiatrist can help you reduce your dosage.
Like other types of anti-anxiety medications, Benzos are potent drugs that may be life-saving in the immediate term if you’ve been taking them for a while. However, there are potential issues and side effects to consider, such as sedation and cognitive difficulties. For many individuals, quitting benzos feels like waking up from a long dream.
Of course, getting out of bed isn’t always simple. Talk to your doctor about the most acceptable way to quit and how you can keep long-term success about your health.
FREQUENTLY ASKED QUESTIONS
Do benzodiazepines have withdrawal signs?
If you follow your doctor’s directions, you should not have any withdrawal difficulties with benzodiazepines if you: use them only once in a while and according to your doctor’s instructions.
However, if you take benzodiazepines regularly and for an extended period, you may become dependent on them. If you quit or decrease your dosage, you may experience physical withdrawal signs or believe that you can’t function in your daily life without them.
What are the symptoms of a benzodiazepine withdrawal addiction treatment?
Symptoms of withdrawal from benzodiazepines may include:
- abdominal cramps, agoraphobia (fear of situations which feel difficult to escape), anxiety, including physical symptoms such as muscle tension, tight chest, fast heartbeat, sweating, trembling, or shaking
- blurred vision, concentration problems, dizziness, face and neck pain, headaches, increased sensitivity to light, noise, touch, and smell, loss of interest in sex, loss of appetite
- mild to moderate depression, nausea (feeling sick), nightmares, panic attacks, restlessness, sleep problems, sore eyes, sore tongue, and metallic taste, tinnitus (ringing in your ears), tingling in the hands and feet (pins and needles), unsteady legs, vomiting (being sick), weight loss.
People who take benzos for a long time may feel more severe symptoms of withdrawal. These might include burning sensations in the skin, confusion, delusions (firmly held beliefs that other people don’t share), depersonalization (feeling detached from your surroundings), derealisation (feeling out of touch with reality), hallucinations, memory loss, muscle twitching, paranoia, seizures (fits).
Stopping abruptly can produce severe withdrawal signs if you’re using benzos regularly. These include confusion, psychosis, seizures, and various symptoms, including a fast heart rate, sweating, high blood pressure, tremor (shaking), hallucination, and agitated behavior.
When might I experience withdrawal from benzodiazepine substance abuse treatment?
Symptoms of withdrawal from a short-acting benzodiazepine can begin several hours after you stop taking it. Alternatively, they might start up to three weeks after you stop utilizing a long-acting benzodiazepine. This is because long-lasting benzos stay in your system for an extended period following their discontinuation. The more time you take benzos, the more difficult it is to quit and the higher your risk of experiencing withdrawal signs. If you’ve been taking short-acting benzodiazepines for a long time, they might be adamant about stopping.
How can I safely stop taking benzodiazepines?
You should gradually decrease your dosage if you stop taking benzodiazepines, which lowers the potential for withdrawal signs. Your doctor can give you further information on how to quit any medicine safely. You may also benefit from speaking with others about your decision. This might be as simple as participating in a local or internet support group or assistance from friends and family.
How do antidepressants help with benzodiazepine withdrawal?
After stopping benzos, some people develop depression. If you’re having trouble coping with the symptoms of depression, your doctor may prescribe antidepressants to help you manage. However, according to some research, selective serotonin reuptake inhibitors (SSRIs) appear to be ineffective in treating depressive symptoms that develop after stopping benzos.
How do benzodiazepines differ from each other?
There are several ways in which benzodiazepines are different from each other:
- Length of half-life
The half-lives of various benzodiazepines vary, and some drugs have a longer duration of action in the brain and body than others. A half-life is a valuable tool for determining how long a drug’s effects will last.
Short-acting benzodiazepines have a shorter half-life, and this means that the medicines are broken down and eliminated from the body faster. Short-acting medications have a greater potential of producing withdrawal signs, and this is because after you stop taking them, your body has less time to adapt to life without them.
Long-acting benzodiazepines have a longer half-life. Because the substances are metabolized more slowly, they stay in your system for longer. When you take these medicines, you are more prone to suffer from a hangover effect, and however, you are less likely to experience withdrawals.
Short-acting benzodiazepines are used as sleeping pills and long-acting benzodiazepines as anxiety medications. However, this isn’t always the case. If you take them at night, some medicines for anxiety can help you sleep. And if you take sleeping pills during the day, lower doses may help you feel calm.
- Potency (strength)
Because different medications are combined in the same pill, the potency of each component varies, and this is due to the strength of the chemical reaction that each drug induces in your body. Taking a smaller dose of a high-potency benzodiazepine may produce similar effects to taking a more significant dose of a low-potency benzodiazepine.
- Metabolization (breakdown in the body)
The body metabolizes benzodiazepines in a variety of ways. This is referred to as your body’s response to the medication. When diazepam is metabolized, extra benzodiazepine chemicals are generated. These extras stay in your system and extend the drug’s effective duration.
Why not give up on benzodiazepines now?
Benzodiazepines are used for short-term treatment because long-term usage might lead to addiction. When you stop taking the drug, withdrawal signs
appear.
Can I take myself off benzodiazepines?
It’s difficult to stop taking medicines on your own, and doing so abruptly can be excruciating. With help from your doctor, it is easier to achieve this. If long-term use of benzodiazepines concerns you, speak with your doctor.
When do symptoms of abrupt withdrawal start, and how long do they last?
Short- and long-acting varieties of benzodiazepines are available. Within a few days, abrupt cessation of short-acting benzodiazepines can cause symptoms. Symptoms from abrupt termination of long-acting benzodiazepines may begin within a week, and symptoms can persist for weeks to months after abruptly stopping benzos.
How can my doctor help?
If you still feel drowsy or need assistance with activities of daily living despite tapering your dosage, it’s time to call your doctor. In tiny increments, your doctor may aid you in lowering your dose and then stopping the medication.
How long will it take?
There are numerous aspects to consider when determining how long it will take to decrease the dosage of a drug and stop taking it altogether. Some people require weeks to reduce their medication dose, while others need months. A physician can assist you in coming up with a strategy that works for you.
Why am I required to take another benzodiazepine to get off it?
Because a long-acting benzodiazepine such as diazepam is more likely to result in a softer reduction, it might help you quit your pill entirely.
What else does it involve?
Your doctor will discuss a withdrawal strategy that is appropriate for you. This may include an agreement on where you can pick up your medicine, how often you should go to the pharmacy, and how to handle any symptoms of withdrawal that may appear.
The best chance of withdrawal success depends on good communication with your doctor.
Remember, people who use benzos can become dependent quickly. Stopping benzodiazepines abruptly may be quite harmful – talk to your doctor first. You will experience withdrawal signs if you stop taking benzos and other prescription drugs.
What else should I know?
Although rare, benzodiazepines may cause a paradoxical reaction that results in aggressive behavior or fearfulness in some people. If this occurs for you, talk to your doctor right away about changing the dosage or using a different medication.
If you’re taking a benzodiazepine with an opioid painkiller, always talk with a medical professional before stopping the opioid. Stopping opioids abruptly may cause serious side effects such as seizures and fatal withdrawal symptoms.
Can I drink alcohol while taking benzodiazepines?
Benzodiazepines and alcohol can interact in some harmful ways. It is best to avoid drinking any alcoholic beverages while on a benzodiazepine, especially if you aren’t sure how your body will react to the combination of drugs. If you must drink, be sure to talk to your doctor about how much you can safely consume.
Can I mix benzodiazepines with other drugs?
Some medications that are safe when taken alone can cause severe problems if they’re combined with benzos. If you need to take another drug, always talk with your doctor first to see if mixing it with a benzodiazepine will cause any problems.
Can I take benzodiazepines with other medications for mental health disorders?
When taken alone, some drugs prescribed to treat mental health conditions are safe when used with benzodiazepines. However, because they can have different effects on your body, you should always talk with your doctor before combining them. If possible, it may be best to take other medications on a different day than you take your benzodiazepine.
What are some lifestyle changes that can help?
There are a few things you can do to make withdrawal less severe. You can take supplements for anxiety and depression or drink chamomile tea to reduce the symptoms. Avoid caffeine, as it will likely worsen your physical symptoms. Try eating small, healthy snacks throughout the day so that you have more energy. Try to eat regular meals whenever possible. Keep yourself busy with work or a hobby outside of the house. Finally, talk about your concerns with a loved one that you trust.
How long does it take for symptoms to improve after I stop taking benzodiazepines?
Most symptoms will begin to improve within a few days, but they may continue for months in some cases. The length of the withdrawal process varies from person to person, but in most cases, it’s approximately six months.
You should contact your doctor immediately if you experience any of the following symptoms:
- Chest pain
- A pounding or racing heartbeat
- Trouble breathing
- Extreme confusion or agitation
- Thoughts of hurting yourself or someone else
What happens to your body as you withdraw from benzos?
As you stop taking benzodiazepines, the chemicals in your brain increase rapidly and become out of balance. This causes the common withdrawal symptoms that you may experience when coming off benzos, and it may take your body some time to readjust to life without benzos.
How long does it usually take for symptoms to improve after I stop taking benzodiazepines?
Symptoms will begin to improve within a few days, but they may continue for months in some cases. The length of the withdrawal process varies from person to person, but in most cases, it’s approximately six months.
What is the difference between benzodiazepines and barbiturates?
Benzodiazepines are medications that slow down brain activity, while barbiturates slow brain activity down to the point of a coma. Benzodiazepines can be addictive if taken with alcohol or opioids, and Barbiturates can be addictive on their own.
What else should I know about benzodiazepines?
Benzodiazepines are medications that slow down brain activity. They’re most often prescribed to treat anxiety, insomnia, seizures, and panic disorders. Benzodiazepines can also reduce muscle spasms and relieve tension caused by alcohol withdrawal or withdrawal from opioids.
What is the difference between benzodiazepines and amphetamines?
Benzodiazepines are medications that slow down brain activity while amphetamines speed it up. Benzodiazepines can be addictive if they’re taken with alcohol or opioids. Amphetamines can’t cause addiction on their own, but if combined with other drugs like opioids, the risk of addiction increases.